As the sun began to rise over the bustling city, Sarah laced up her sneakers and stepped out for her morning jog. For her, this was more than just a workout; it was a way to reclaim her health after receiving a life-altering diagnosis: diabetes. At first, the news felt overwhelming. The word “diabetes” conjured up images of needles, dietary restrictions, and endless blood sugar checks, but it all started with a few vague diabetes symptoms she hadn’t recognized at the time. Yet, Sarah was determined to learn everything she could about her condition and finally take control of her life again.
Like Sarah, many people find themselves navigating the complexities of diabetes, whether it’s type 1, a condition often diagnosed in childhood, or type 2, which is increasingly common among adults. The reality is that diabetes affects millions of individuals worldwide, each facing their unique challenges and journeys. It can be daunting, but understanding what diabetes is, its causes and the treatment options available can empower individuals to manage their health effectively.
In this comprehensive guide, we’ll explore the essential aspects of diabetes. We’ll explain what diabetes is, highlight the differences between type 1 and type 2, show you how healthcare providers diagnose it, and break down common diabetes symptoms, treatment options, and more. Whether you’ve just received a diagnosis, are helping a loved one, or simply want to learn more, this guide will give you clear, practical information to support your journey. We aim to provide you with valuable insights and resources for navigating life with diabetes.
What is Diabetes?
Diabetes is a chronic health condition that affects how your body turns food into energy. Our bodies break down most of the food we eat into sugar (glucose) and release it into the bloodstream. When your blood sugar rises, it signals your pancreas to release insulin, a hormone that helps cells absorb sugar from the bloodstream to use as energy. In diabetes, this process doesn’t work properly, leading to high blood sugar levels, which can cause a range of health problems over time.
There are two main types of diabetes: Type 1 and Type 2. Though they share some similarities, they differ in how and why they develop.
Type 1 Diabetes Symptoms
Type 1 diabetes, also known as insulin-dependent diabetes, is an autoimmune condition. In this form of diabetes, the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, people with Type 1 diabetes are unable to produce insulin, and they must take insulin daily to survive.
Type 1 diabetes can develop at any age, but doctors most commonly diagnose it in children, teens, and young adults. Researchers haven’t fully uncovered the exact cause, but they believe a combination of genetic factors and environmental triggers, like viruses, plays a role.
Symptoms of Type 1 Diabetes:
- Increased thirst and frequent urination
- Unintended weight loss
- Extreme hunger
- Fatigue and weakness
- Blurred vision
Since Type 1 diabetes is an autoimmune condition, it cannot be prevented. Managing the condition requires daily insulin administration, monitoring blood sugar levels, and making lifestyle adjustments.
Type 2 Diabetes Symptoms
Type 2 diabetes is the most common form of diabetes and typically develops later in life. However, doctors are diagnosing it more frequently in younger individuals, including children and teens. In Type 2 diabetes, the body still produces insulin, but it either doesn’t use it efficiently (a condition called insulin resistance) or doesn’t produce enough insulin to maintain normal blood sugar levels.
Type 2 diabetes is largely linked to lifestyle factors, such as poor diet, lack of physical activity, and obesity, although genetics also play a significant role. Early diabetes symptoms like fatigue, frequent urination, and increased thirst often go unnoticed until the condition progresses. People can often prevent or delay Type 2 diabetes by making healthy lifestyle choices, unlike with Type 1 diabetes.
Symptoms of Type 2 Diabetes:
- Frequent urination, especially at night
- Excessive thirst
- Unexplained weight loss
- Fatigue
- Slow-healing sores or frequent infections
- Tingling or numbness in the hands or feet
Managing Type 2 diabetes often involves lifestyle changes such as eating a healthy diet, exercising regularly, and maintaining a healthy weight. Some people may also need medication or insulin to help manage their blood sugar levels.
Gestational Diabetes Symptoms
While Type 1 and Type 2 are the most well-known forms of diabetes, it’s also important to mention gestational diabetes, which develops during pregnancy. This condition affects how your cells use sugar and can pose risks for both mother and baby if not properly managed. Although gestational diabetes usually goes away after pregnancy, it increases the risk of developing Type 2 diabetes later in life.
Differences Between Type 1 and Type 2 Diabetes Symptoms
Type 1 and Type 2 diabetes both affect how the body processes glucose, but they differ in their causes, diabetes symptoms, treatment approaches, and the groups of people they typically affect. Understanding these distinctions is essential for managing each type effectively and for raising awareness about how the conditions differ.
Cause and Onset
Type 1 Diabetes:
Autoimmune Condition: In Type 1 diabetes, the immune system mistakenly attacks the insulin-producing cells in the pancreas (beta cells). Over time, this leads to a complete lack of insulin production.
No Known Prevention: Since it’s an autoimmune disorder, Type 1 diabetes cannot be prevented. Genetics play a role, but environmental triggers (like viral infections) are also thought to contribute.
Typically Early Onset: Type 1 diabetes is most often diagnosed in childhood, adolescence, or young adulthood, though it can develop at any age. Symptoms tend to appear suddenly and may escalate quickly.
Type 2 Diabetes:
Insulin Resistance: Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas doesn’t produce enough insulin to keep blood sugar levels normal. Over time, the body’s ability to produce insulin can also decrease.
Largely Preventable: Lifestyle factors like poor diet, lack of exercise, and obesity are key contributors to the development of Type 2 diabetes. However, genetic predisposition also plays a role.
Gradual Onset in Adults: Type 2 diabetes typically develops later in life, often in middle age or beyond. However, rising obesity rates have caused doctors to diagnose more cases in younger people, even in children. Symptoms usually develop gradually and may go unnoticed for years.
Insulin Dependence
Type 1 Diabetes:
Completely Insulin-Dependent: People with Type 1 diabetes cannot produce insulin. As a result, they must take insulin daily. Either through injections or an insulin pump, to survive. Without insulin, blood sugar levels can become dangerously high, leading to life-threatening complications.
Type 2 Diabetes:
May Not Require Insulin Initially: Many people with Type 2 diabetes can manage their condition through lifestyle changes. Diet and exercise are often the first steps toward better blood sugar control. In some cases, doctors prescribe oral medications to help the body use insulin more effectively. However, as the disease progresses, some people with Type 2 may eventually need insulin to manage their blood sugar levels.
Risk Factors
Type 1 Diabetes:
Family History: Having a close relative with Type 1 diabetes increases your risk. However, it’s not as strongly inherited as Type 2 diabetes.
Environmental Triggers: Research suggests that certain viruses or environmental factors may trigger the autoimmune response that leads to Type 1 diabetes, but the exact cause remains unclear.
Type 2 Diabetes:
Lifestyle Factors: Unhealthy habits are major contributors to the development of Type 2 diabetes. These include being overweight, eating a diet high in sugars and processed foods, and leading a sedentary lifestyle.
Genetics: A strong family history of Type 2 diabetes significantly increases your risk.

Diabetes Symptoms and Detection
Type 1 Diabetes:
Rapid Symptom Onset: Symptoms such as extreme thirst, frequent urination, weight loss, and fatigue can develop rapidly over the course of a few weeks. Because the pancreas stops producing insulin almost completely, blood sugar levels can skyrocket quickly, leading to diabetic ketoacidosis (DKA), a life-threatening condition if untreated.
Type 2 Diabetes:
Gradual Symptom Onset: Symptoms of Type 2 diabetes, such as fatigue, frequent urination, blurred vision, and slow healing of cuts or sores, often develop slowly and may be mild at first. This can make it harder to diagnose in the early stages. Some people may not realize they have diabetes until they develop complications like nerve damage or cardiovascular problems.
Management
Type 1 Diabetes:
Lifelong Insulin Therapy: Because Type 1 diabetes is an autoimmune condition, people with it must use insulin therapy for life. They need to carefully monitor their blood sugar levels and regularly adjust their insulin doses based on their diet, activity levels, and overall health.
Type 2 Diabetes:
Lifestyle and Medication Management: While insulin therapy may be needed later in life for some people with Type 2 diabetes, it’s not always the first line of treatment. In the early stages, the condition is often managed through lifestyle changes like healthy eating, regular physical activity, and weight loss. Oral medications that help the body respond to insulin are also commonly used.
Prevention
Type 1 Diabetes:
No Prevention: As an autoimmune disease, there are currently no known ways to prevent Type 1 diabetes. Early diagnosis and proper management are critical to prevent complications.
Type 2 Diabetes:
Preventable with Lifestyle Changes: In many cases, people can prevent or delay Type 2 diabetes by maintaining a healthy weight, eating a balanced diet, exercising regularly, and avoiding smoking and excessive alcohol use. Taking action early is critical for managing prediabetes, a condition where blood sugar levels are elevated but haven’t yet reached the threshold for a diabetes diagnosis.
Diagnosis and Treatment Options
Diagnosing diabetes typically involves a combination of medical history, physical examinations, and specific blood tests. The following are the standard tests used to diagnose both type 1 and type 2 diabetes:
- Fasting Plasma Glucose Test: This test measures blood sugar levels after fasting for at least eight hours. A fasting blood sugar level of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): After fasting overnight, blood sugar is tested, and then the patient drinks a sugary solution. Blood sugar levels are tested again two hours later. A result of 200 mg/dL (11.1 mmol/L) or higher indicates diabetes.
- Hemoglobin A1c Test: This test provides an average blood sugar level over the past two to three months. An A1c level of 6.5% or higher indicates diabetes.
- Random Plasma Glucose Test: A blood sample is taken at a random time, regardless of when the patient last ate. A glucose level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes.
- C-peptide Test: This test measures the level of insulin produced by the pancreas and can help distinguish between type 1 and type 2 diabetes.

Treatment Options for Diabetes
The treatment for diabetes aims to effectively manage blood sugar levels, address diabetes symptoms, and prevent complications. Treatment plans may vary depending on whether a person has type 1 or type 2 diabetes.
Type 1 Diabetes Treatment
Type 1 diabetes is an autoimmune condition requiring lifelong management, primarily through insulin therapy. Treatment options include:
- Insulin Therapy: Since the pancreas produces little to no insulin in type 1 diabetes, patients need to take insulin injections or use an insulin pump. The types of insulin include:
- Rapid-acting insulin: Starts working within minutes and lasts a few hours.
- Short-acting insulin: Takes longer to start working but lasts longer than rapid-acting.
- Intermediate-acting insulin: Covers insulin needs for about half a day or overnight.
- Long-acting insulin: Provides coverage for a full day or longer.
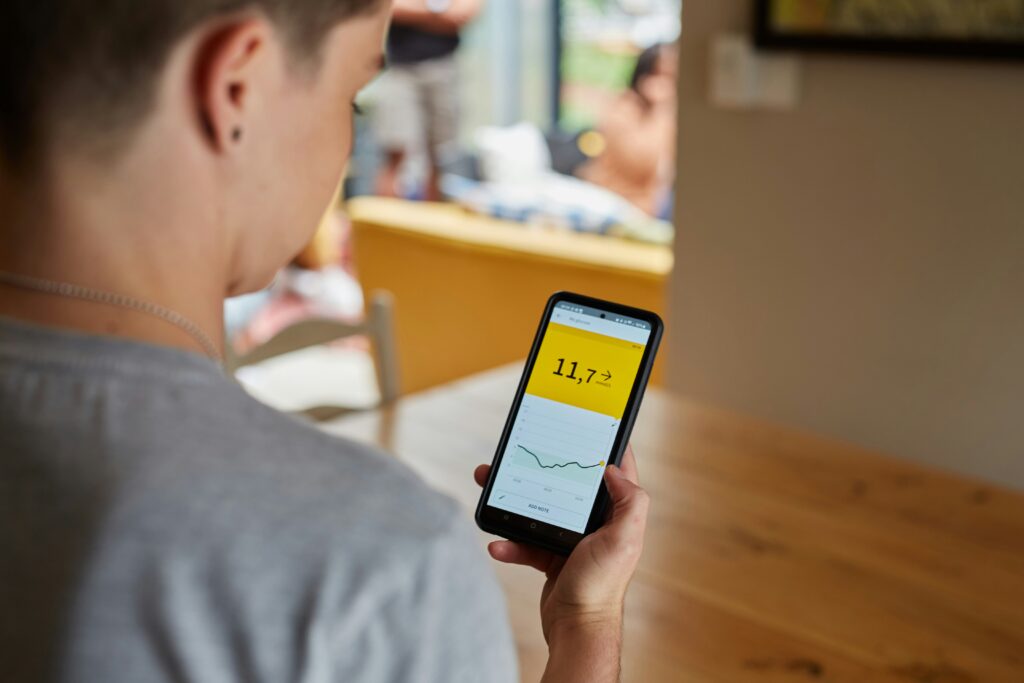
- Continuous Glucose Monitoring (CGM): This technology provides real-time blood sugar readings and alerts patients of highs and lows, helping them manage insulin doses more effectively.
- Healthy Lifestyle Choices: Individuals are encouraged to maintain a balanced diet, exercise regularly, and monitor their blood sugar levels.
Type 2 Diabetes Treatment
Type 2 diabetes is often managed through lifestyle changes, but medication may be necessary. Treatment options include:
- Lifestyle Modifications: The first line of defense for type 2 diabetes involves making changes to diet and physical activity levels. This includes:
- Following a balanced diet low in refined sugars and high in fiber.
- Engaging in regular physical exercise (at least 150 minutes per week).
- Losing weight if overweight, as even a small percentage of weight loss, can improve insulin sensitivity.
- Oral Medications: Various oral medications can help control blood sugar levels, including:
- Metformin: Reduces glucose production in the liver and increases insulin sensitivity.
- Sulfonylureas: Stimulate the pancreas to produce more insulin.
- DPP-4 inhibitors: Help reduce blood sugar levels without causing weight gain.
- SGLT2 inhibitors: Help the kidneys remove glucose from the bloodstream.
- Insulin Therapy: Some individuals with type 2 diabetes may eventually need insulin therapy, especially if their blood sugar levels remain high despite oral medications.
- Monitoring Blood Sugar Levels: Regular self-monitoring of blood sugar levels is crucial for all diabetes patients, allowing for timely adjustments to treatment plans.
- Regular Check-Ups: Routine visits with healthcare providers to monitor overall health and manage any complications are essential.
Understanding the diagnosis and treatment options for diabetes empowers individuals to take an active role in their health and work with healthcare professionals to develop a personalized management plan.
Living with diabetes, whether type 1 or type 2, is a journey that requires ongoing education, management, and support. By understanding the nature of the condition, recognizing common diabetes symptoms, and knowing the available treatment options, individuals can take significant steps toward effectively managing their health.
Staying informed about diabetes empowers you to make educated choices that can improve your quality of life and help prevent complications. Remember, you’re not alone on this journey; there are abundant resources and communities ready to support you.
To stay updated with the latest information, tips, and support for managing diabetes, sign up for our newsletter! Join our community and receive valuable insights straight to your inbox, helping you stay informed and empowered on your path to health.

Leave a Reply
You must be logged in to post a comment.